Breast Implant Explantation in Elderly Patients
Post-augmentation pain is a common occurrence, especially among patients who underwent breast augmentation more than a decade ago. Even when facing complications such as breast firmness, recurrent ptosis, implant malposition, capsular contracture, pseudocapsule formation, implant displacement, symmastia, tight pocket, or unsightly scarring, many women continue to endure discomfort due to psychological burden, compounded by age-related surgical concerns in which patient safety is a primary criterion.
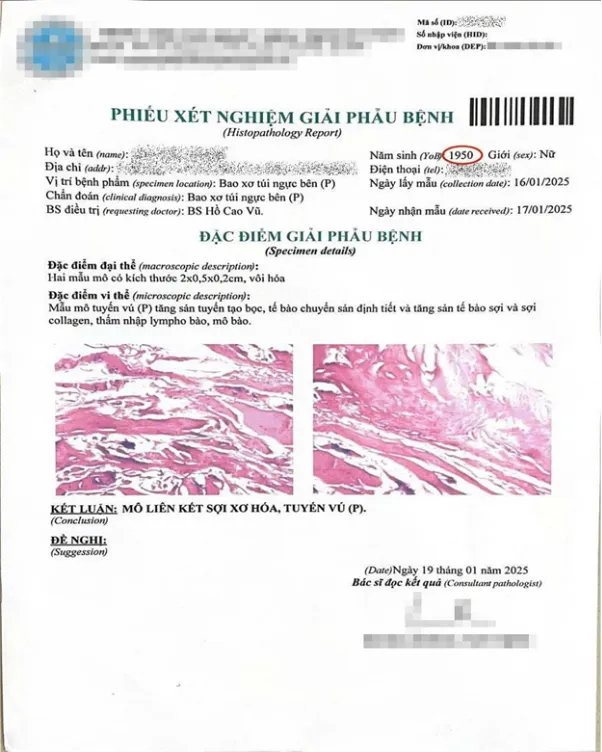
Histopathological result of a 75-year-old patient after explantation and capsulectomy
According to MD, MSc. Ho Cao Vu, who has performed over 1,000 breast explantation procedures: "Many patients over the age of 50 hope for painless explantation, minimal downtime, and preservation of systemic health, particularly in the presence of comorbidities such as diabetes, hepatic disorders, thyroid dysfunction, coagulation disorders, cardiovascular disease, or hypertension."
Potential intraoperative complications in elderly patients include: hemorrhage, pulmonary embolism, respiratory failure, myocardial infarction, deep vein thrombosis—factors that adversely affect wound healing and postoperative recovery. Therefore, choosing a surgical technique that limits hemorrhage, performed in a general hospital licensed by the Department of Health with adequate infrastructure, equipment, qualified surgical teams, and emergency resuscitation capabilities, is imperative.

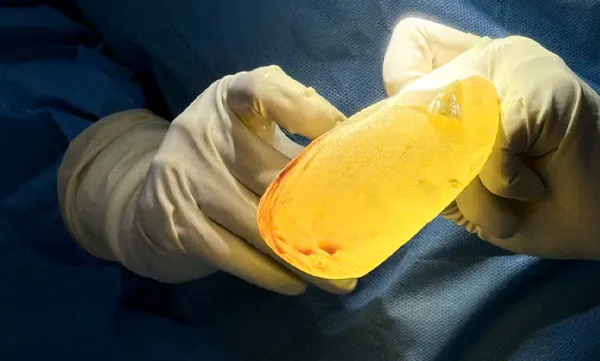
Explanted ruptured textured implant after 10 years
Patient concerns following breast implant explantation
1. Is breast implant explantation painful?
Breast implant explantation is a major surgical procedure, requiring standard preoperative evaluation and intraoperative protocols. In explantation cases utilizing ultrasonic surgical scalpel, there is no intraoperative hemorrhage, and soft tissue trauma is minimized. When combined with laryngeal mask airway (LMA) anesthesia or intravenous general anesthesia, patients can typically be discharged within 4 hours postoperatively.
2. What is the postoperative recovery time?
In most cases where ultrasonic surgical scalpel are applied, patients do not require no postoperative downtime, do not require suture removal, and can resume daily activities shortly after anesthetic recovery. This method offers significant advantages for patients who are hesitant to undergo surgery or live far from the facility, allowing them to return to daily life within 4 hours.
3. What will breasts look like after explantation?
Post-explantation outcomes depend on skin elasticity, degree of dermal aging, internal glandular tissue, implant size, and condition of the implant pocket. The timing and extent of breast retraction vary from patient to patient.
4. When is implant replacement appropriate?
In elderly patients desiring re-implantation, consultation with an experienced surgeon is essential to determine the most appropriate implant pocket creation techniques to ensure long-term stability (over 20 years), implant size selection appropriate for age and body structure, and a surgical approach that ensures minimal trauma, hemorrhage while maintaining safety.

Explantation of Ruptured Allergan Gel Implant
Explantation Procedure Using Laryngeal Mask Airway Anesthesia
Laryngeal mask airway (LMA) anesthesia offers significant advantages for both adult and pediatric patients. This technique is not only easy to manage for surgeons and anesthesiology staff but also significantly reduces the risk of laryngeal trauma during the procedure. Moreover, LMA causes less airway irritation, resulting in smoother emergence from anesthesia and a lower incidence of side effects compared to endotracheal intubation.
In standard explantation procedures, MD, MSc. Ho Cao Vu utilizes laryngeal mask airway anesthesia in combination with an ultrasonic surgical scalpel, resulting in no hemorrhage, no tissue damage, and an atraumatic explantation technique.
Postoperatively, patients experience no pain, require no postoperative downtime, are discharged within 4 to 6 hours, and do not need any analgesics or antibiotics after surgery. For these reasons, the anesthesiology team unanimously agreed that laryngeal mask airway anesthesia provides superior patient safety and comfort both during and after breast implant explantation.

The patient underwent explantation of Motiva implants six years after augmentation, presenting with recurrent breast ptosis.
Safety Is the Top Priority in Breast Implant Explantation Surgery
For elderly patients with multiple comorbidities, a full panel of multi-organ function tests must be conducted at general hospitals with comprehensive specialty departments. Additionally, the surgical facility must have an ICU that meets emergency resuscitation standards, and a team of experienced physicians capable of managing intraoperative complications such as anaphylactic shock, myocardial infarction, and thrombosis. The following preoperative tests are mandatory for patients undergoing breast implant explantation:
1. Complete Blood Count (CBC): To assess red blood cells, white blood cells, and platelet levels, helping detect anemia or infection.
2. Liver and Renal Function Tests: Including AST, ALT, creatinine, BUN, and estimated glomerular filtration rate (eGFR), to ensure the liver and kidneys are functioning properly and can effectively metabolize and eliminate anesthetic agents.

Explantation of textured implants after 15 years of augmentation.
3. Coagulation profile (PT, APTT, INR): Evaluates the patient’s blood clotting capacity to reduce the risk of hemorrhage during and after surgery.
4. Blood glucose test (Glucose): Screens for or monitors diabetes, as impaired glucose control can negatively affect wound healing.
5. Electrocardiogram (ECG), chest X-ray, and echocardiography: Assess pulmonary and cardiac function to ensure no respiratory compromise or underlying cardiovascular conditions prior to anesthesia.
6. Implant evaluation (for explantation cases): MRI and ultrasound to assess for implant rupture, leakage, or deformation; evaluate pocket thickness, soft tissue defect location, and associated complications.
7. Chronic disease screening: In cases of comorbidities such as hypertension, diabetes, or autoimmune disorders, additional specialized tests (e.g., HbA1c, immunologic assays) may be required.
Tags:





